Baby Gut Health Protocols: A Prevention Guide for Midwives, Parents, and Healthcare Workers
Antibiotics don’t “just pass through”—they strip butyrate production for months
🧭 WHO THIS IS FOR:
Midwives
Doulas
NICU nurses
Pediatricians ready to break ranks
New parents
Community birthworkers
Any health worker watching diagnosis rates rise and feeling helpless
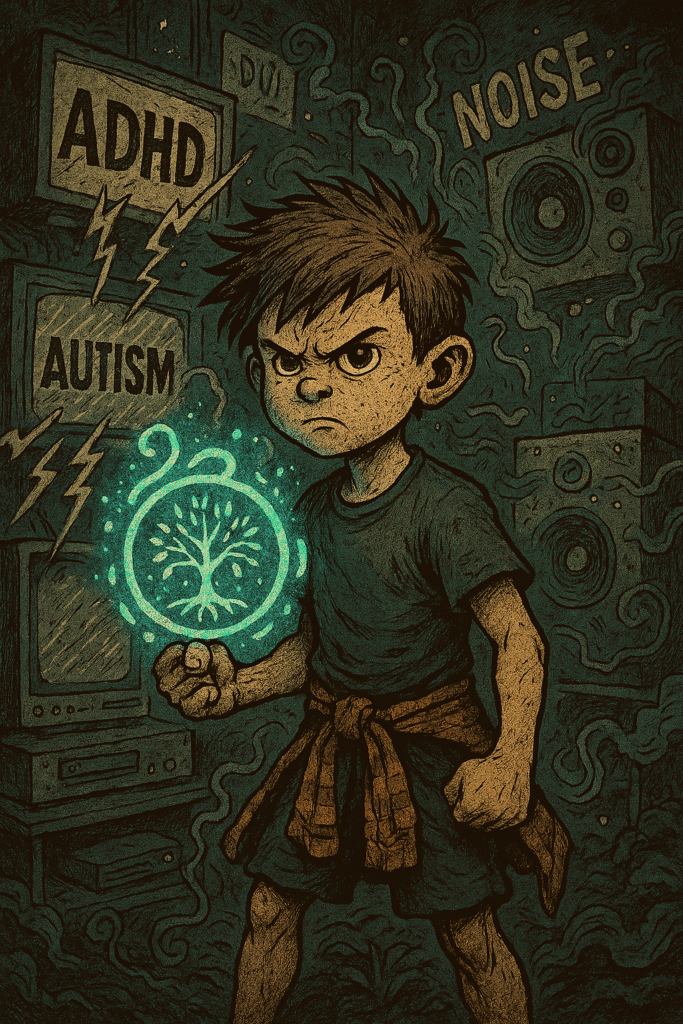
🔓 WHAT YOU WEREN’T TOLD IN TRAINING:
C-sections aren’t neutral—they come with microbial cost
Formula feeding isn’t sterile—it’s inflammatory terrain for many
Antibiotics don’t “just pass through”—they strip butyrate production for months
Vaccine reactions are terrain-dependent (especially in dysbiotic kids)
Developmental delay often follows a microbial wipeout event—and nobody tracks it
You were taught protocol.
Not ecology.
Not terrain.
Not gut-time bombs disguised as pediatric norms.
Now we rebuild.
🌱 PREVENTION STARTS IN THE WOMB
👶 For pregnancy + birth prep:
Avoid antibiotics unless absolutely necessary
Use diet-based prebiotics (green banana, lentils, fiber) to support maternal gut
Encourage natural birth whenever safe
Avoid excessive glyphosate and synthetic food intake
Supplement with gentle gut support (e.g. fermented foods, herbal teas)
🍼 IF BIRTH INTERVENTIONS OCCUR:
No shame. Just recalibrate.
In case of C-section:
Use vaginal seeding (if safe and informed)
Begin microbial terrain support ASAP
Avoid antibiotics unless life-threatening
Consider:
Infant-safe prebiotic drops
Spore probiotics (low dose, infrequent)
Breast milk or donor milk (if possible)
Introduce polyphenols via mother’s milk (pomegranate, coriander, etc.)
💉 POST-VACCINE TERRAIN CARE:
Again—not anti-vax, not dogma. Just gut-first support.
Delay vaccines slightly in:
Children with active gut issues
Recent antibiotic use
Known regressions post-immune triggers
Use herbal calming support post-vax:
Coriander seed tea
Butyrate if tolerated
Slippery elm or marshmallow for gut repair
💊 ANTIBIOTIC RECOVERY PROTOCOL (INFANTS & TODDLERS)
Stop emulsifiers and processed foods
Introduce resistant starch (e.g. green banana flour)
Support mucus repair:
Marshmallow root, colostrum (if tolerated), ghee
Pulse in spore probiotics (tiny doses)
Introduce butyrate slowly if GI inflammation is low
Use fermented food brine if histamine issues are not present
🧪 WHAT TO TRACK INSTEAD OF DIAGNOSIS:
Gut regularity + stool consistency
Sleep patterns
Language bursts or stalls
Social engagement shifts
Emotional volatility post-medication or food changes
Skin conditions, histamine responses
Signs of neuroinflammation: dilated pupils, toe walking, hand flapping, zoning out
Most of these happen before diagnosis ever lands.
And most of them happen when the Trio is already gone.
The “Muddy Middle” — and Real Life
📣 THE CALL TO CARE WORKERS
You are the firewall.
Not after the diagnosis.
Before it.
We don’t need a new drug.
We need a generation of nurses, doulas, midwives, and herbalists who understand this:
If the gut terrain is intact, the mind has a chance.
If the Trio survives, the child has options.
If the inflammation is prevented, the spectrum may not manifest.
You are not powerless.
You are the gatekeeper now.
